Fibromyalgia: Symptoms, Root Causes, Types of Pain, Diagnosis & Treatment!

Fibromyalgia: Symptoms, Causes, Diagnosis & Treatment!
What is Fibromyalgia, and What fibromyalgia means?
Fibromyalgia or Fibromyalgia Pain Syndrome is an idiopathic (meaning without a known cause) disease. Fibromyalgia is a chronic and widespread musculoskeletal pain and fatigue disorder with generalized tender points.
It is a multisystem disease, and fibromyalgia symptoms are long-term, body-wide pain in muscles, ligaments, and tendons – the soft fibrous tissues in the body. Other fibromyalgia symptoms are sleep disturbance, restless sleep, awakening feeling tired, morning stiffness, fatigue, headache, anxiety, depression, and irritable bowel syndrome (IBS).
According to the National Institutes of Health (NIH), fibromyalgia affects an estimated 5 to 6 million Americans.
Fibromyalgia word comes from the Latin term for fibrous tissue (fibro) and the Greek words for muscle (myo) and pain (algia). People with fibromyalgia indeed endure widespread, chronic muscle discomfort.
The main symptoms of fibromyalgia (FM) are widespread chronic pain, unrefreshing sleep, physical exhaustion, and cognitive difficulties. Fibromyalgia was formerly classified as an inflammatory musculoskeletal disease but is now considered an illness primarily affecting the central nervous system. Scientists do not fully understand what causes fibromyalgia, but people with the disorder have a heightened pain sensitivity.
Management of patients who describe fibromyalgia symptoms as chronic pain all over the body, associated with sleep disturbance, overwhelming fatigue, alteration in mood, or psychological distress that worsens the quality of their life is often complex and challenging. As a result, this syndrome has been named by terms such as “neurasthenia,” “fibrositis,” and “fibromyalgia.”
Fibromyalgia typically starts in middle age, and fibromyalgia symptoms in females are more common and intense, but it can also strike men and people of all ages, including children. In addition, people with autoimmune conditions like lupus or rheumatoid arthritis are more prone to the disorder than the general population.
Fibromyalgia is a common rheumatologic disorder that is underdiagnosed. The prevalence of fibromyalgia in the general population of the United States is reported to be 5.00 percent in women and 0.5 percent in men. Most fibromyalgia symptoms increase steadily through 80 years of age and then decline. Fibromyalgia symptoms in females are observed ten times more often than in men. Fibromyalgia is usually considered a disorder of women 20 to 50 years of age; however, it also has been observed in males, children, adolescents, and older persons. Fibromyalgia is more common in relatives of patients with fibromyalgia, suggesting the contribution of genetic and environmental factors.
What Causes Fibromyalgia?
It is yet unknown what causes fibromyalgia; hence the condition is considered idiopathic. Why fibromyalgia occurs, and the cause of fibromyalgia remains somewhat of a mystery. This chronic condition is thought to be caused by an error in how your brain processes pain. Lower levels of neurotransmitters such as serotonin or norepinephrine can cause feelings of fibromyalgia symptoms such as fatigue or exaggerated pain.
The truth is that what causes fibromyalgia is unknown. Still, it’s thought to be related to abnormal levels of certain chemicals in the brain and changes in how the central nervous system (the brain, spinal cord, and nerves) processes pain messages throughout the body.
It’s also suggested that some people are more likely to develop fibromyalgia because of genes inherited from their parents.
In many cases, the symptoms of fibromyalgia appear to be triggered by physical or emotional things like an injury, infection, or stress.
Is Fibromyalgia an Autoimmune Disease?
Fibromyalgia is not an autoimmune disease. However, it does accompany other autoimmune rheumatic and endocrine disorders. As per scientific research, fibromyalgia is a neurological disease affecting a person’s sensory processing system. Fibromyalgia does not involve inflammation or damage to joints. Instead, brain imaging and studies have shown fibromyalgia is a central nervous system disorder.
Are Fibromyalgia and Neuropathy Related?
The Mystery Deepens Fibromyalgia with Small Fiber Neuropathy. The current research provides further evidence that fibromyalgia is essentially a neurological disorder.
There is evidence of nerve damage in about half of fibromyalgia patients. According to a study from Massachusetts General Hospital (MGH), researchers published in the eminent journal PAIN found that almost half of a group of patients with fibromyalgia — a common syndrome that causes chronic pain and other symptoms — was found to have damage to nerve fibers in their skin and other evidence of a disease called small-fiber polyneuropathy (SFPN).
Unlike fibromyalgia, which has had no known causes and few effective treatments, small-fiber polyneuropathy has a clear pathology. In addition, it is known to be caused by specific medical conditions, most of which can be treated, cured, and reversed.
Fibromyalgia and Small Fiber Neuropathy: The Plot Thickens! These new findings support fibromyalgia as a primarily neurological entity, nevertheless.
Potential Connections Between Fibromyalgia and Small-Fiber Peripheral Neuropathy!
Nerve Damage and Fibromyalgia:
Researchers at Harvard-affiliated Massachusetts General Hospital found that half of the sufferers of fibromyalgia symptoms have damage to nerve fibers in their skin and other evidence of a disease called small-fiber polyneuropathy. The discovery is vital to finding better treatments.
It is commonly seen that people with symptoms of fibromyalgia often suffer from peripheral nerve damage as well. However, it has also been seen that many patients with both conditions may also have symptoms of diabetes, such as tiredness, loss of energy, soreness, and muscle aches.
In addition, peripheral neuropathy pain in the lower extremities may also be comparable to diabetes based on the tingling, sharp pains, and burning sensations associated with this type of neuropathy: foot neuropathy.
The causes and locations of pain experienced by people with diabetic neuropathy and fibromyalgia are very different. But despite these apparent differences, both entities have similar abnormal sensory complaints and pain qualities. Recent research hypothesized that similar sensory symptoms might be associated with similar mechanisms of pain generation. This opens the possibility of focusing on treatment strategies for patients suffering from fibromyalgia symptoms.
A scientific study has linked the pain of fibromyalgia to small nerve fiber neuropathy, which is painful damage to a specific part of a particular nerve. This could be a ground-breaking study, as fibromyalgia has previously been linked to nerve dysfunction but not to actual nerve damage.
What Fibromyalgia Feels Like, or What Fibromyalgia Pain Feels Like?
Tactile Allodynia: One of the symptoms of fibromyalgia is a hypersensitivity to touch or tactile allodynia. It’s a neurological disorder that causes mild or even light touches to seem like stabbing agony. Tactile stimuli that would typically do no damage are experienced as painful when this syndrome is present.
Things that don’t usually cause pain can be very painful. These may include cold temperatures, brushing hair, or wearing a cotton t-shirt.
Fibromyalgia can make you extremely sensitive to pain all over your body, and you may find that even the slightest touch is painful. In addition, if you hurt yourself, such as stubbing your toe, the pain may continue for much longer than it usually would.
The main symptoms of fibromyalgia are chronic, widespread pain throughout the body or at multiple sites. Fibromyalgia pain is often felt in the arms, legs, head, chest, abdomen, back, and buttocks.
People often describe it as aching, burning, or throbbing. However, it is mainly felt at fibromyalgia pain points: Lower neck in front, edge of upper breast, arm near the elbow, knee, base of the skull in the back of the head, hip bone, upper outer buttock, back of the neck, and back of the shoulders.
Fibromyalgia symptoms in females are more intense and painful at fibromyalgia pain points.
Is Fibromyalgia an Actual Medical Condition, or Is it All in One’s Head?
The short answer to this query is that fibromyalgia is an actual medical condition, and fibromyalgia symptoms make its patients’ daily life miserable. About four to five million Americans have fibromyalgia. It’s a syndrome characterized by fibromyalgia symptoms like persistent pain that may have its origins in nervous system dysfunction. The medical world is now unanimous in accepting fibromyalgia as a real disorder.
Using magnetic resonance imaging (MRI), scientists have discovered anomalies in the region of the brain responsible for processing pain signals in persons with fibromyalgia symptoms. It appears that this brain segment amplifies the intensity of normal standard signals, standard signals using the body to feel pain without a physical cause.
When the Fibromyalgia Pain is Severe, gets Worse and Causes Fibromyalgia Flare-Ups?
Fibromyalgia pain usually becomes severe or worse, or fibromyalgia flares up when the fibromyalgia patient is under stress, exhaustion, poor sleep, dietary shifts, hormone disruptions, and environmental factors all have a role in the development of fibromyalgia symptoms. In addition, giving birth, getting hurt or sick, having major surgery, experiencing significant life changes, or grieving can all bring on a fibromyalgia flare-up.
Fibromyalgia flares-ups are characterized by symptoms similar to the flu, such as body aches and tiredness, discomfort, and lethargy.
In fibromyalgia patients, a flare is a temporary increase in the number or severity of fibromyalgia symptoms. Attacks might last anywhere from a few days to a few weeks.
Fibromyalgia symptoms may worsen if you’re exposed to something to which you’re allergic. Symptoms of fibromyalgia in women are more severe, with debilitating pain.
What is Fibrofog?
Fibrofog, also known as fibromyalgia fog and brain fog – is a common way to describe the brain-related problems that can occur with fibromyalgia. Scientists don’t yet fully understand its causes and effects, but treating sleeping problems, depression, fatigue, and chronic pain improves symptoms.
Fibrofog is a term coined by patient support groups to describe cognitive complaints associated with fibromyalgia. Dr. Glass, an eminent scientist, explained that patients with symptoms of fibromyalgia experience a decrease in memory, loss of vocabulary, and a lack of concentration, which are exacerbated in stressful work environments.
What Causes Fibrofog?
What Causes Fibro Fog? Scientists don’t know for sure. Some experts theorize that fibro fog may be related to the impact of fibromyalgia symptoms, particularly pain at fibromyalgia pain points. Managing chronic pain demands attention and may require mental effort, which can reduce available cognitive processing resources and affect performance on a cognitive task.k
Why does Fibromyalgia also Causes Fatigue?
One theory for why fibromyalgia also causes fatigue is that fatigue is the result of your body trying to deal with the pain. Fibromyalgia fatigue doesn’t go away even after sleep or rest. This constant reaction to pain signals in your nerves can make you sluggish and exhausted. People with fibromyalgia frequently also have trouble sleeping (insomnia).
According to the National Fibromyalgia Association, fibromyalgia affects between 3 and 6 percent of people worldwide.
Why does Fibromyalgia also Cause Anxiety?
The high correlation between fibromyalgia and anxiety may stem from the two having some physiological underpinnings. For example, Serotonin and GABA problems, among others, have been associated with both.
Malfunctioning Neurotransmitters: Chemical signals between brain cells are transmitted by neurotransmitters. The neurotransmitters serotonin and gamma-aminobutyric acid (GABA) regulate several essential functions of the brain. Anxiety and fibromyalgia are associated with low activity levels of both substances—for example, stress.
Is Fibromyalgia Hereditary?
Although there is no clear genetic link between parents and offspring with fibromyalgia, the condition does seem to run in families. In families where someone with fibromyalgia is a close relative, the risk of having the disorder is several times higher than in families where no one has the ailment.
Fibromyalgia tends to run in families, and some scientists believe specific genes could make you more likely to develop it. However, the disorder also occurs in people with no family history of the disease.excruciating

Why Are Women More Prone to Fibromyalgia?
Women are nine times more likely to develop fibromyalgia syndrome (FMS) than males. Fibromyalgia symptoms in females are characterized by widespread pain and tenderness to the touch (tender spots). Two recent studies highlight substantial disparities in FMS clinical features across sexes. Fibromyalgia symptoms in women like weariness, morning fatigue, aches all over, the overall number of symptoms, and irritable bowel syndrome was considerably more common in women in both the community and clinic samples.
Fibromyalgia pain points or tender spots were noticeably more common in women. There was no significant difference in pain intensity or physical functioning between the sexes, and neither were there any differences in psychological characteristics like stress, anxiety, or depression.
Why fibromyalgia affects much more women than men: Hormonal shifts and the possibility of increased stress due to menstruation, menopause, or pregnancy may put women at a higher risk. The female physiological response to stress is sometimes more intense than the male physiological response. Long-term stress can weaken the immune system, making it less effective at preventing illness.
Women with fibromyalgia symptoms may also feel worsened with lower abdominal and back discomfort due to premenstrual syndrome issues.
Who Gets Fibromyalgia and What are the Risk Factors for Fibromyalgia?
Anyone can get fibromyalgia, but more women get it than men. Fibromyalgia can affect people of any age, even children, but it usually starts in middle age, and the chance of having it increases as you get older. It occurs in people of all racial and ethnic backgrounds.
In the United States, estimates suggest that between 2% to 8% of the population is affected; that’s around 5–10 million adults.
Likely Causes of Fibromyalgia!
If you have other diseases, especially rheumatic diseases, mood disorders, or conditions that cause pain, you may be more likely to have fibromyalgia. These diseases include:
►Rheumatoid arthritis.
►Systemic lupus erythematosus (commonly called lupus).
►Depression and anxiety.
►Chronic back pain.
►Family history
►Irritable bowel syndrome.
►Osteoarthritis.
►Obesity
►Illness (such as viral infections)
►Ankylosing spondylitis.
►Stressful or traumatic events, such as car accidents, post-traumatic stress disorder (PTSD)
►Repetitive injuries. Injury from repetitive stress on a joint, such as frequent knee bending.
►Gender: Women are more likely to have fibromyalgia than men. Some research suggests that up to 90% of sufferers are indeed women.
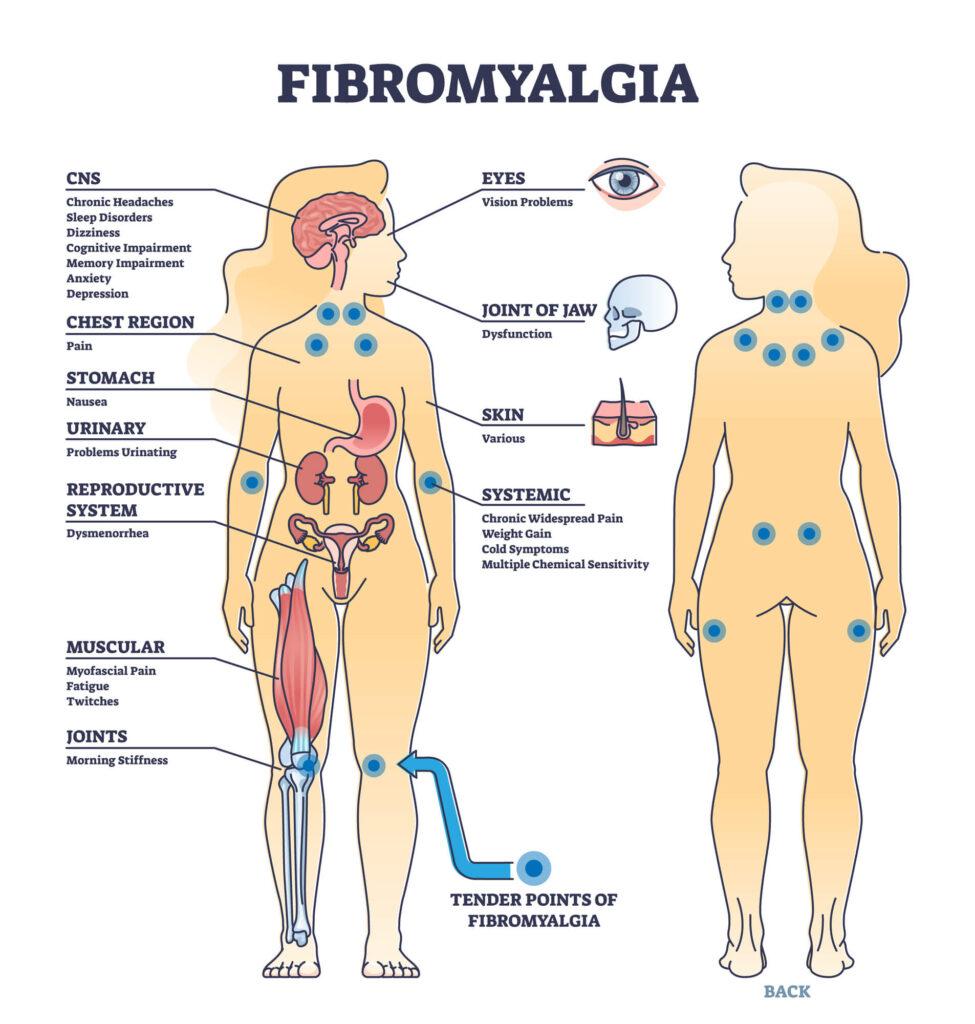
What
are Fibromyalgia Pain Points or Tender Points?
The 18 tender points associated with
fibromyalgia occur in symmetrical pairs from the back of your head to your
inner knees. Following are the main pain points or tender points of the 18
tender points:
►Back of the shoulders.
►Back of the neck,
►Lower neck in front,
►Edge of upper breast,
►Upper outer buttock,
►Base of the skull in the
back of the head,
►Arm near the elbow,
►Hip bone,
►Knee,
What
are 8 Types of Fibromyalgia Pain?
►Allodynia: Experiencing
pain from a stimulus that typically would not, such as a very light touch, is
an example of allodynia.
►Temporomandibular joint
pain (TMJ): TMJ pain is felt in jaw joints and surrounding muscles &
ligaments (headaches, earaches, and facial pain).
►Hyperalgesia: Intense
pain perception is referred to as hyperalgesia.
►Widespread muscle pain
and fatigue
►Neuropathic pain
►Headaches
►Pain in the face
►Abdominal and pelvic pain
What are the Symptoms
of Fibromyalgia?
There may be periods
when your symptoms get better or worse, depending on stress levels, weather
changes, and how physically active you are.
Widespread
pain: One
of the main symptoms is likely widespread pain. This may be felt
throughout your body but could be worse in fibromyalgia
pain points or tender points. The pain could feel like: an
ache, a burning sensation, a sharp, stabbing pain.
Fatigue:
Fibromyalgia
can cause tiredness. This can range from mildly tired to the exhaustion often
felt during a flu-like illness.
Severe tiredness
(fatigue) may come on suddenly and can drain you of all your energy. If this
happens, you may feel too tired to do anything.
Stiffness:
Fibromyalgia
can make you feel stiff. The stiffness may be most severe when you have been in
the same position for an extended period – for example, when you
first wake up in the morning.
Poor
Sleep Quality: Insomnia
is a common symptom of fibromyalgia. Sleep disturbances and feeling exhausted
even after a whole night’s rest are common symptoms.
Because of this fibromyalgia
symptom, you may not be able to get the restful sleep you need. This type of
sleep is sometimes referred to as “non-restorative” sleep.
Extreme
Sensitivity: Fibromyalgia
can make you extremely sensitive to pain all over your body, and you may find
that even the slightest touch is painful.
You may have hyperalgesia
– when you’re extremely sensitive to pain and allodynia – when you
feel pain from something that should not be painful, such as a very light touch.
You may also be
sensitive to smoke, certain foods, and bright lights.
Tension,
Headaches, and Migraine: If fibromyalgia has caused you to experience pain and
stiffness in your neck and shoulders, you may also have frequent headaches.
Depression
& Anxiety: One
of the main symptoms of fibromyalgia is depression.
Constantly feeling down, hopeless and helpless and losing interest in
activities that used to bring you joy are all indicators of depression.
Cognitive
Problems (fibro-fog): Problems with mental processes, such as thinking
and learning, are known as “cognitive disorders.” These are some of
the symptoms you might experience if you have fibromyalgia: difficulty
retaining information and picking up new skills
Problems
with memory, focus, and concentration; sluggish or muddled speech.
Irritable
bowel syndrome (IBS) Some
people with fibromyalgia also have irritable bowel syndrome (IBS). IBS is
a common digestive condition that causes pain and bloating in your stomach. It
can also lead to constipation or diarrhea.
Does Fibromyalgia Affect
Your Eyes?
Fibromyalgia can be
associated with ocular symptoms (foreign body sensation, irritation) and visual
disturbances (blurred vision), coexisting with dry eye syndrome, and reduced
corneal sensitivity.
Additional
Fibromyalgia Symptoms:
In addition to the
pain, people living with fibromyalgia may also experience dizziness,
clumsiness, difficulty controlling their body temperature (leading to
uncomfortable extremes of heat and cold), and an intense need to exercise their
legs (restless legs syndrome) constantly.
Pins and needles,
also known as paraesthesia, are sensations of tingling, numbness, prickling, or
burning in the hands and feet—stiffness in the limbs and numbness in the arms
and legs. One of the fibromyalgia symptoms in females is painful periods.
Rare
Symptoms of Fibromyalgia
1. Brain Fog: This frustrating illness, sometimes known as “fibro
fog,” is a primary cause of mental suffering. Cognitive impairments result
from impaired focus and memory. Patients suffering from brain fog frequently
complain of memory recall issues and the ability to think, pay attention, and converse.
They can also rely on their short-term memory. According to medical
professionals, factors including illness and lack of sleep contribute to the
onset of brain fog.
2. Paresthesia: Paresthesia is a condition characterized by a
burning or prickling feeling, most commonly affecting the extremities. The
sudden onset of a sensation has been described as tingling, numbness, skin
crawling, or itching.
3. Allodynia: Neuropathic pain is known as allodynia (nerve
pain). Those who suffer from allodynia have an abnormally high response to
touch. The pain from something that wouldn’t usually hurt might be
excruciating. Using a hairbrush, a relaxed environment, or a cotton t-shirt
could fall into this category.
4. Extreme Sweating: It’s not uncommon for people with fibromyalgia
to sweat so much that it gives the impression that they have a fever. The
hypothalamus, a small area of the brain that controls autonomic functions and
links the nervous and endocrine systems, is to blame for this disorder. That
means it keeps things like sleep and perspiration at a steady temperature,
among other automatic biological processes.
5. Sound and Smell Sensitivity: It is thought that fibromyalgia patients also
experience this latent symptom, which is linked to allodynia. Increased
sensitivity to smells and sounds is a common symptom of fibromyalgia. On rare
occasions, they may also experience light sensitivity.
Those with
fibromyalgia have a heightened response to environmental stimuli like light,
smell, and sound. This is why problems like headaches, dizziness, and nausea
can manifest physically after experiencing too much sensory stimulation.
6. Dystonia: Dystonia is characterized by recurring,
rhythmic, and involuntary twitches of the muscles. Because of this, you can engage
in behaviors like twisting your body in a circular motion. Dystonia is
classified as segmental if it affects three or more joints, focal if it affects
only one, and generally if it affects the complete body (general dystonia).
7. Lipomas: Lipomas are rare tumors that can affect
anyone. One should also remember that having fibromyalgia does not make one
more susceptible to these ailments. Accumulations of subcutaneous fat, while
unsightly, provide no health risks.
Who Diagnose and Treats
Fibromyalgia?
Fibromyalgia is a difficult-to-diagnose
disorder with a wide range of symptoms of fibromyalgia that affect the quality
of life.
Rheumatologists are
internal medicine doctors focusing on diagnosing and treating conditions
affecting the body’s musculoskeletal and connective tissue systems, including
arthritis. Rheumatologists, perhaps more than any other type of doctor, keep up
with research on fibromyalgia, and as a result, they have the most
comprehensive understanding of the disorder. Unfortunately, not all
rheumatologists are well-versed in fibromyalgia and its manifestations.
Neurologists diagnose
and treat conditions related to the brain and spinal cord. In the same way that
only some rheumatologists are knowledgeable about fibromyalgia, many
neurologists also need a thorough understanding of the condition. When you
visit a neurologist, it is usually because of the discomfort associated with
fibromyalgia.
Specialists in pain
management can help with various conditions, including fibromyalgia. It’s essential
to verify that your chosen pain management facility treats fibromyalgia before
making an appointment. But many specialists in pain management are qualified to
address the condition.
Finding a doctor who
understands fibromyalgia may take time, but don’t get discouraged. You can
manage and treat your symptoms of fibromyalgia right in your home.
How is Fibromyalgia Diagnosed,
or How Can I Tell If I Have Fibromyalgia?
Fibromyalgia is an
idiopathic disease, meaning without a known cause, doctors diagnose
fibromyalgia based on all the patient’s relevant symptoms (what you feel), no
longer just on the number of tender places during an examination. There was no
test to detect this disease, but you may need lab tests or X-rays to rule out
other health problems.
According to a recent
scientific article in The American Academy of Family Physicians Foundation, the
FM/a Test is a blood test used to diagnose fibromyalgia. It is available for
use in patients of any age with at least four typical symptoms of fibromyalgia.
The FM/a Test is a
blood test used for the diagnosis of fibromyalgia. It is available for use in
patients of any age with at least four typical symptoms of fibromyalgia.
What
is the Best Fibromyalgia Diet?
Some dietary modifications have been shown to help
patients with fibromyalgia, a chronic pain illness that can be difficult to
manage. Although the specifics of the best fibromyalgia diet that may assist
vary from person to person, some have found relief by reducing their diet of
food allergens and gluten and increasing their consumption of anti-inflammatory
foods like antioxidant-rich vegetables and fish.
For more information on the
fibromyalgia diet, kindly click here.

Affiliate Disclosure “If you buy through links on our site, we may earn an affiliate commission, no worries though, you’ll still pay the standard amount so there’s no cost on your part. However, please know this does not impact our reviews and product information. We try to keep things fair and balanced to help you make the best choice for your needs. This keeps it 100% reader-supported and free of advertisements or sponsorships. Thanks for your support!”
Medical Disclaimer:
All content and media on this Website are created and published
online for informational purposes only. It is not intended to be a substitute
for professional medical advice and should not be relied on as health or
personal advice.
Always seek the guidance of your doctor or other qualified
health professional with any questions you may have regarding your health or a
medical condition. Never disregard the advice of a medical professional, or
delay in seeking it because of something you have read on this Website.